Covid Hospital Rescue
By Rebecca Terrell
Prior to the Covid crisis, hospitals were viewed as harbors of safe refuge. Now, many see them as little more than prison wards, where patients can be isolated from their families, deprived of informed consent, and robbed of reasonable alternative treatments to dictates handed down by Washington bureaucrats.
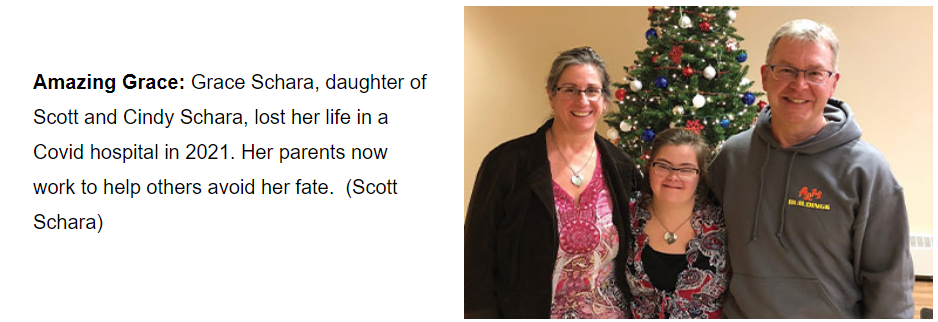
Scott Schara lives daily with the tragedy that brought him to that conclusion. His daughter, Grace, died on October 13, 2021 in a Covid hospital in Wisconsin and is now counted among the more than 1.1 million U.S. Covid deaths tallied by the Centers for Disease Control and Prevention. But Scott blames a genocidal hospital agenda with profit as its goal — not Covid — for the death of his youngest daughter.
“Grace was my best buddy,” he remembers. She was 19 years old and had Down syndrome. “If anyone knows someone with Down syndrome, you know that they’re your best buddy.”
Scott describes Grace as having been “super high functioning.” Not only could she read and write, but she could also drive a car, ride horses, play the violin, compose beautiful works of art, and crack jokes that would leave a room in stitches.
“This mission is because of her,” he told The New American, referring to his commitment to helping others avoid her fate. “Whenever you lose somebody, especially somebody like Grace, you don’t want their death to be in vain.”
He now reaches thousands through his website, OurAmazingGrace.net, as well as regular newsletters and a podcast called “Deprogramming with Grace’s Dad.”
“We know of hundreds of people directly — because they contact us — that Grace’s death has saved,” Scott said.
But last November, he showed his true mettle as the hero in a “hospital hostage situation” in his own back yard.
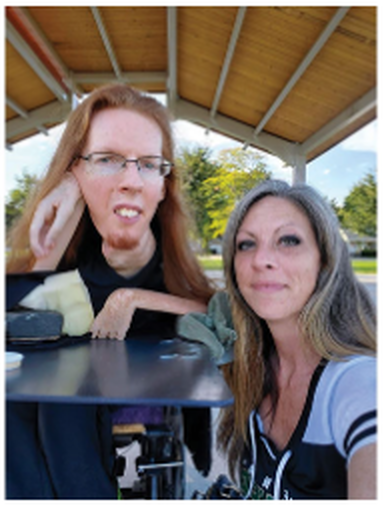
Robert’s Story
Last November, a woman called Scott and introduced herself as Heather. She had seen the billboards Scott placed in the vicinity of Green Bay, Wisconsin, warning people about what had happened to his beloved daughter.
“Can you help me?” he remembers her asking. He inquired what was going on.
“My brother is in a hospital in Green Bay, and he’s disabled.” She went on to explain that her brother, Robert Paiser, has a condition called SMA, or spinal muscular atrophy, a rare genetic and degenerative disorder that leaves its victims with progressively declining muscle mass. At 44 years of age, Robert weighs only 40 pounds and is confined to a wheelchair, though he is extremely intelligent and able to talk. He had contracted a flu and was being treated in the hospital.
“Heather, this is going to sound strange, and you’re going to think that I’m crazy, but they are going to try to kill him,” Scott told her. But the same reality had already occurred to Heather, hence her call.
“What do I do?” she asked.
“You’ve got to be in that hospital as an advocate to save his life,” Scott implored, “not to be there to hold his hand so he doesn’t get lonely, but literally to save his life.”
Scott went through a list of imperatives with Heather: no DNR (do not resuscitate) order, no remdesivir (the government-approved anti-viral drug for treating Covid-19), no ventilator, and no jabs. “You have to lay the law down. None of those things for your brother,” he emphasized.
Heather took Scott’s advice and went straight to the hospital. The next day, she texted him that Robert had already been given remdesivir.
“I got ahold of her as fast as I could,” Scott recalls, “because this suddenly went from urgent to an emergency.” He said that his research shows that three doses of remdesivir translate to a 75-percent chance of death. Indeed, the 2019 PALM Clinical Trial terminated remdesivir early because more than half of patients who consumed the drug during testing had died, and because researchers noted extensive kidney damage in survivors. However, it is the only medicine with Food and Drug Administration approval for Covid treatment.
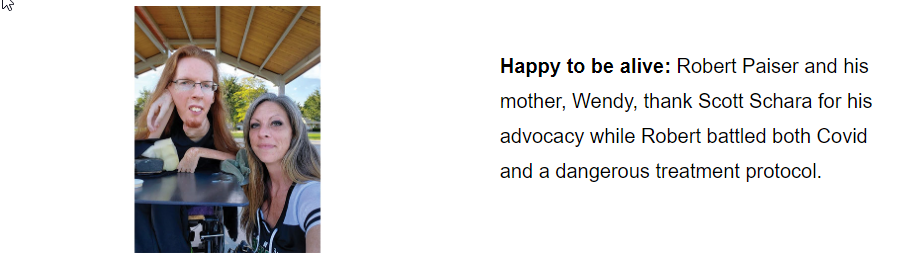
Heather relayed these facts to Robert, who until that point had trusted his doctor to look out for his best interests. His faith shaken and his health rapidly deteriorating, Robert asked Scott to come to the hospital to advocate for him.
During this back-and-forth, Scott reached out to three friends who are experienced in hospital rescues. Nicole Landers with the Truth For Health Foundation; Laura Bartlett, founder of the Hospital Hostage Hotline; and Greta Crawford, founder of ProtocolKills.com jumped into action.
“They did some coaching with me and got me a medical directives form,” he said, and he rushed to the hospital with that life-saving paperwork.
“Please Don’t Leave Me!”
“You know, when you get to a setting like this, you don’t know what to expect,” Scott pointed out. “But I was able to walk right into the room.”
What he saw took his breath away. Robert was lying near death, and Scott could not help but recall his own bitter experience with the loss of Grace.
“I got down next to him, and I gave him a hug,” Scott remembers. “I prayed with him, and he looked me in the eye and said, ‘Scott, please don’t leave me!’”
“I won’t,” was the tearful response.
Scott says Robert could still talk, but “he was in bad shape.” He had already been given three doses of remdesivir, but considering his body weight, “it was the equivalent of six doses.”
“I thought he was going to die,” admits Scott. Despite his emaciated condition, Robert was extremely bloated from excess fluid. Heather told Scott that the hospital refused to feed Robert, instead making his family bring food from home. “It was terrible care,” Scott said. “They wouldn’t even bathe him or let him sit up in bed.”
Scott started going through the medical directives form with Robert and his family. Robert agreed to all of the “imperatives” Scott had delineated for Heather earlier. As Robert’s power of attorney, she signed the forms, and they called a meeting with the doctor.
“The doctor comes in in this whole space suit contraption, really showing Robert this is a fearful situation,” Scott relates. “He’s got a mask on, he’s got a shield on,” and he was wearing a beard net. They reviewed the medical directives with him, and Scott says that the next time the doctor entered the room later that day, all the protective garb was gone. “The gig was up,” he surmised.
Meanwhile, Scott also focused on saving Robert’s life. He phoned Dr. Peter McCullough, once vice chief of internal medicine at Baylor University Medical Center who was one of the first doctors to advocate for proven, successful alternative treatments for Covid. Dr. McCullough put Scott in touch with Dr. Paul Marik, co-founder of the Front Line COVID Critical Care Alliance. Within minutes, Dr. Marik was on the phone walking Scott through exactly what to do for Robert.
“He gave me the dosages for ivermectin, NAC [N-acetyl cysteine], vitamin D, vitamin C, zinc, and then he said, ‘Get a budesonide treatment,’” Scott recalls. But where could he get all of that in the hospital at a moment’s notice?
Scott called his wife, Cindy, at home, and told her to bring his personal supplies. “How am I going to do that?” Cindy asked, incredulously. “How am I going to hide it?”
“You can just walk right in,” he assured her. In a short time, she arrived. By then, Scott and Heather had made sure that Robert was bathed, and Scott said they started administering Dr. Marik’s suggested treatment. “The doctor did one thing in Robert’s favor,” says Scott. “He prescribed budesonide, so we were even able to give him that.”
Within what seemed a miraculously short time, Robert began to improve. “He started to turn around, and we watched the man become alive right before our eyes,” Scott exults. But the adventure was not yet over.
“Unbelievably, even though we had been through that directives form with the doctor and the nurse, another nurse came in the room to give Robert the Covid flu jab!” Scott relates, still incredulous. “It wasn’t enough they gave him six doses of remdesivir. They want to kill him with the jab!”
That was, of course, refused, and Robert soon received a second budesonide treatment, at which point he decided, in Scott’s words, “Let’s get out of here!” The doctor would not dismiss him, so Robert decided to leave “against medical advice” (AMA), which is a term for hospital discharge prior to doctor-sanctioned release. AMA is acknowledged to be a patient’s right, but Scott said the hospital staff refused to remove Robert’s intravenous (IV) line. Only after a shift change could he find a nurse willing to remove the IV.
As they were departing, Scott turned to a nurse. “I may never have this opportunity again, so I’d like to ask you a question. I just want to know, why would you do this? You know they’re trying to kill him. Why would you participate?”
She did not acknowledge that the hospital wanted to kill Robert, but her response dismayed Scott. “I’m from the Philippines,” he recalls her reply. “And if I don’t do exactly what they say, they will deport me.”
Combating the Agenda
Scott believes Covid hospitals are targeting disabled individuals such as Grace and Robert, first of all because their deaths bring in massive government payoffs courtesy of the 2020 Coronavirus Aid, Relief and Economic Security Act and add-on payments from the Centers for Medicare & Medicaid Services (CMS). Those measures are still in effect since President Biden has extended the Covid public health emergency, though he admitted during a televised interview last September that “the pandemic is over.”
The other motive, Scott believes, is to dispose of individuals considered to be a burden on the CMS system. He cites the Center for Infectious Disease Research and Policy at the University of Minnesota, which reported that “intellectual disability is second only to old age as a risk factor for COVID-19 death.” One study found that those with intellectual disability risked higher chances of dying from Covid than did those with congestive heart failure, kidney disease, or lung disease. Other research reveals that in “New York, the state with the most deaths from COVID-19, people with developmental disabilities die at a rate 2.5 times the rate of others who contract the virus.”
Scott also points to a 2021 Medicare Trustee’s Report, which notes the high cost of federally funded care for the elderly and disabled and calls for “substantial changes” to address financial challenges. Scott believes these changes involve planned genocide that is turning hospitals across the country into “the new killing fields.”
“Before Grace died, I trusted the white coat,” he told The New American. “I fell for the Covid propaganda.” Grace’s death opened his eyes, and he believes Robert and many others are alive today because of his own tragic loss. He views his role of patient advocate as a gift from God that allows his “amazing” Grace’s light to shine on.
Published with permission of thenewamerican.com