How to Avoid the Leading Cause of Disability
Analysis by Dr. Joseph Mercola Fact Checked
STORY AT-A-GLANCE
- Back pain is one of the most common health complaints across the globe and the No. 1 cause of job disability
- Chronic back pain is also one of the most common reasons for opioid dependence, the side effects of which can be lethal. In fact, opioids are now the leading cause of death among Americans under the age of 50. Up to 25% of opioid users also end up with other substance-abuse disorders
- Research shows you can successfully reverse chronic back pain by retraining your brain to appropriately respond to nerve signals gone haywire through a technique called Pain Reprocessing Therapy (PRT). PRT helps “rewire” neural pathways such that pain is deactivated
- Staying active and minimizing sitting are two strategies that can go a long way toward preventing — and treating — back pain. Both will improve muscle strength and coordination, reduce stiffness and improve blood flow, which may reduce back pain and lower your risk of developing back pain in the first place
- Other nondrug treatment alternatives for back pain include strategies addressing improper body mechanics, such as the Gokhale Method, Foundation Training and Neurostructural Integration Technique (NST), and chiropractic adjustments, acupuncture, massage, compression breathing, stretching and techniques that address repressed emotions
Back pain is one of the most common health complaints across the globe, with an estimated 80% of people experiencing back pain at some point in their life.1 Not only is back pain the No. 1 cause of job disability,2 it’s also one of the most common reasons for opioid dependence, the side effects of which can be lethal. In fact, opioids are now the leading cause of death among Americans under the age of 50.3
According to a 2018 study,4,5 opioids — which modulate your brain’s reaction to pain — are the most commonly prescribed medications for people with chronic low back pain and, as you’d suspect, these drugs are typically used long-term in this population.
According to Pharmacy Times, about 20% of patients on long-term opioid therapy end up developing an opioid use disorder.6 Up to 25% of opioid users also end up with other substance-abuse disorders,7 which have additional risks.
The use of opioids for back pain flies in the face of guidelines8 from the American College of Physicians, which recommends heat wraps and exercise as a first line of treatment, stressing that prescription drugs should only be used as a last resort, as they completely fail to treat the underlying problem.
Research9 has also shown opioids (including morphine, Vicodin, oxycodone and fentanyl) fail to control moderate to severe pain any better than over-the-counter (OTC) drugs such as acetaminophen, ibuprofen and naproxen. In fact, those taking nonopioid pain relievers actually fared “significantly better” in terms of pain intensity.
Considering the immense risks associated with opioid use, you’d be wise to exhaust all other alternatives before jumping on that bandwagon to disaster. The good news is there are a wide variety of non-drug options available.
Unlearning Chronic Back Pain
Most recently, researchers have shown you can successfully reverse chronic back pain by retraining your brain with Pain Reprocessing Therapy (PRT).10 As reported by DW.com:11
“PRT aims to rewire neural pathways in the brain to deactivate pain and train the brain to respond to signals from the body more appropriately, using what’s called pain education. Ultimately, the goal is to reduce a patient’s fear of certain movements, so that when they do move in those ways, they are confident that it won’t cause them any pain.”
The article tells the story of one of the study participants, Daniel Waldrip, who had suffered chronic debilitating back pain for 18 years. One month after the conclusion of the study, Waldrip was 100% pain free, and he’s remained pain free in the four years since. “It completely changed my life,” he told DW.com.
Pain Processing Gone Haywire
If pain can be “unlearned,” what does that say about the nature of pain? Contrary to popular belief, chronic back pain is not always due to some structural or mechanical problem. More often than not, it’s actually caused by nerves sending incorrect or faulty signals to your brain. As explained by DW:12
“Pain is like an alarm system that alerts us when we may have hurt ourselves or become injured. But regardless of where a person hurts themselves physically, their sense of pain is formed in the brain.
Nerves send signals to the brain to let it know that something has happened in the body and the brain then decides whether to produce a pain sensation, and that depends on whether the brain thinks there is danger.
Pain draws a person’s attention to potential harm and diminishes when that warning signal is no longer needed. This is called acute pain … But pain that persists for more than three months despite treatment is considered chronic.
‘It’s really important that people are able to experience pain. It’s critical for survival, and yet some people [continue to have] pain even though their bodies have recovered,’ said James McAuley, a psychologist and professor at the University of New South Wales (UNSW).
While scientists have their theories, it is still unclear what causes chronic pain or how acute pain becomes chronic, said McAuley. But they do know that some changes occur in the brain when pain goes from acute to chronic.
‘The nerves are misfiring and advising the brain that the patient is having pain or is at a risk of damage,’ said Steven Faux, director of the Rehabilitation Unit at St Vincent’s Public Hospital in Sydney, Australia.”
In all, two-thirds of the volunteers in the PRT group were either pain free or nearly pain free at the end of the treatment, compared to just one-fifth (20%) of those in the placebo group. Functional MRI scans performed at baseline and at the end of the trial also demonstrated that pain processing in the brain had been noticeably altered.
The Importance of Staying Active and Minimizing Sitting
Staying active and minimizing sitting are two strategies that can go a long way toward preventing — and treating — back pain. Both will improve muscle strength and coordination, reduce stiffness and improve blood flow, which may reduce back pain and lower your risk of developing back pain in the first place.
Oftentimes, back pain originates from tension and muscular imbalances. For example, sitting for long periods of time ends up shortening the iliacus, psoas and quadratus lumborum muscles that connect from your lumbar region to the top of your femur and pelvis.
When these muscles are chronically short, it can cause severe pain when you stand up as they will effectively pull your lower back (lumbar) forward. By bringing these muscles into better balance, you will remedy many of these common pains and discomforts.
This was certainly true for me when I had debilitating back pain about 10 years ago that failed to respond to all interventions. The only thing that worked was to stop sitting for over 12 hours a day. I shifted to a standing desk and the problem permanently resolved: Address the cause and you typically have a cure.
Overuse and misuse of the muscles supporting your spine, poor muscle strength and inappropriate posture while sitting, standing and walking are other common causes of low back pain. For instance, when walking with your toes pointed outward, the muscles in your hips and lower back tighten, increasing your risk for lower back pain.
Sitting with your shoulders hunched over a computer screen stretches muscles in your upper back and places added stress on your lower back, increasing your risk for both lower and upper back pain.
Walking with your head down is yet another posture-related problem that has repercussions on the rest of your back and hips,13 as your head is the single heaviest part of your body and will throw everything out of alignment. If poor posture is a culprit, consider doing some exercises to stretch out your shoulders, open up your hip flexors, and lift your chest.
Correct Improper Body Mechanics That Cause Pain
Techniques that can ease or erase back pain by teaching you proper body mechanics include:
- Foundation Training,14which helps strengthen your core. This includes anything that directly connects to your pelvis, whether above or below it. Foundation Training teaches all those muscles to work together through integrated chains of movement, which is how your body is structurally designed to move.
- Neurostructural integration technique(NST), a gentle, noninvasive technique that stimulates your body’s reflexes. Simple movements are done across muscles, nerves and connective tissue, which helps your neuromuscular system to reset all related tension levels, promoting natural healing.
To learn more, you can download Michael Nixon-Livy’s free ebook,15 “Neurostructural Integration Technique: A Better Way to Good Health” from nsthealth.com. Basic training videos are also available on Vimeo.16 To find an NST therapist near you, see our NST Therapists Page.
- The Gokhale Method,17which helps restore your structural integrity by sitting, standing and moving correctly.
Benefits of Chiropractic Care
Spinal adjustment by a chiropractor can also ease back pain in many cases. In one 2017 meta-analysis18 of 26 studies, spinal manipulation was associated with “statistically significant benefits in both pain and function, of on average modest magnitude, at up to six weeks.”
The average patient reported greater ease and comfort in their day-to-day activities, such as walking, sleeping or turning in bed. However, while these results appear to be modest in nature, it is important to recognize the results are an average, and that the participants only underwent manipulation. In other words, they were not given any additional rehabilitative exercises designed to maintain functional movement of the spine gained after manipulation, or to reduce inflammation.
A study19,20 that did take physical therapy and/or anti-inflammatories into account, published in 2018, found this kind of multidisciplinary approach reduced discomfort and disability to a greater than standard medical care.
In all, 750 active duty military service members already being treated for lower back pain were evaluated. All were receiving physical therapy and/or drugs to ease pain and inflammation. The team added chiropractic treatment to half the participants, including spinal manipulation, rehabilitation exercises and treatment with cold or heat.
On average, the chiropractic treatment group received two to five treatments over a six-week period. After six weeks, patients who received chiropractic treatments experienced greater improvements in their lower back pain and less disability than those who did not receive the treatments. Lead study author and chiropractor Christine Goertz, Ph.D., commented on the results:21
“Spinal manipulation (often referred to as Hias chiropractic adjustment) may help heal tissues in your body that form as a result of injury, decreasing pain and improving your body’s ability to move correctly.
It is also possible that manipulation impacts the way your body perceives pain through either the brain or spinal cord and or decreases pain from muscle strain, inflammation and or spasm in the muscles next to your spine.”
Aside from addressing any immediate spinal misalignment that might cause back pain, chiropractic care can also help address, prevent and treat deeper dysfunctions in your body. Chiropractic adjustments can actually affect the chemistry of biological processes on a cellular level, thereby reducing oxidative stress and improving immune function and DNA repair,22 for example.
Acupuncture and Massage
Acupuncture and massage also have their place, and often work well together. The WellBridge Clinic in Oregon is a proponent of acupuncture for back pain, stating on its website:23
“There is extensive, conclusive research behind the use of acupuncture for pain resolution and management, especially for back pain. Modern science has found that targeting specific points in the body with acupuncture pins acts as a nociceptive stimulation that leads to the activation of the nerve-endocrine-immune systems.
This activation helps the body to begin to heal at the sites of injury and pain. Effectively, this means it increases blood flow and circulation to injured areas. It changes the electrical current that is the foundation of our biology. That’s how acupuncture releases endorphins to ease pain, release muscle tension, and change cellular processes so the body can heal.”
Back problems that may respond well to acupuncture include pinched nerves, sciatica, herniated discs and spinal stenosis. Massage therapy, meanwhile, releases endorphins that help induce relaxation, relieve pain and reduce levels of stress chemicals such as cortisol and noradrenaline. It also reverses the damaging effects of stress by slowing your heart rate, respiration and metabolism, and lowering high blood pressure.
Benefits of Compression Breathing
Certain breathing techniques can even be helpful. Compression breathing is actually an important aspect of Foundation Training. It helps re-educate the muscles surrounding the spine of your rib cage, teaching them to be in a state of expansion rather than contraction. This technique is demonstrated in the video above.
Done properly, it will help lengthen your hip flexors, stabilize your spine and support your core using transverse abdominal muscles. This strengthens your back and keeps your chest high and open — all of which can reduce pain. Here’s a quick summary of how to do structured decompression breathing:
- Whether sitting down or standing, put your thumbs at the base of your rib cage, positioning your pinkies at the pointy bones at the front of your waist. Think of the space between your fingers as a measuring stick.
- Pull your chin back so your chest is lifting upward. Take three slow deep breaths as instructed below.
- The distance between your thumbs and pinkies should increase as you breathe in.
- When you breathe out, tighten your abdominal muscles so your torso will not collapse back down. This is the most important step: Do not let your torso drop back down toward the pelvis as you exhale. It should be challenging, allowing you to feel your abdomen engage as you exhale.
- With each breath, your aim is to increase the distance between your thumb and pinky fingers, as well as increase the width of your upper back. This occurs as you elongate the back of your rib cage. Each inhalation expands your rib cage, and each exhalation will keep the abdomen extended and tight. So, each in-breath fills up your rib cage, and each out-breath maintains the height and width of your rib cage.
Repeat five to 10 rounds with three to four breaths per round. Over time, your muscles will get stronger and your seated posture will gradually improve.
Simple Stretches to Help Relieve Lower Back Pain
Stretching is also important, as tight and stiff muscles and lack of flexibility will contribute to back pain. There are many options here. Below, I’ve highlighted six simple stretches commonly recommended for lower back pain.24 The Yoga Journal25 also has an online page demonstrating poses that can be helpful.
If these stretches are too painful to perform, stop doing them and consult your doctor, chiropractor or massage therapist before continuing. You may experience mild discomfort when you begin doing these stretches, especially if you are new to exercise or it has been a long time since you last exercised. My advice is to take it slowly and gradually increase your tolerance to these stretches over time.
- Baby Cobra —Lie on your stomach with your legs together, arms bent and palms on the ground at chest level, elbows bent. Inhale and lift your chest, keeping the back of your neck long and your chin relaxed. Exhale and return your forehead to the mat. Repeat a few times, focusing on your breath.
- Bird dog —Begin on all fours, then lift and extend one leg and the opposite arm at the same time. Hold for three to five breaths. Switch sides and raise and hold the opposite arm and leg for three to five breaths.
- Cat/cow —Begin on all fours. Place your hands directly under your shoulders and your knees under your hips. On your inhalation, drop your belly and lift your gaze up to the ceiling. When you exhale, round your spine so your tailbone drops between your thighs and your head lifts between your arms. Repeat multiple times, slowly, to gently increase spinal mobility.
- Psoas lunges —Your psoas muscle extends from your lowest vertebrae to the top of your thigh, putting it in a good position to stress your lower back when it becomes tight. A great way to stretch your psoas is through lunges.
Begin by standing on your knees. Bring your right leg in front of you so that your right foot is on the floor and your knee is bent at a 90-degree angle. Tuck your buttocks slightly and place your hands on your right knee, or your hips. Allow your hips to gently shift forward as you breathe for three to five breaths. Repeat on the other side.
- Twist —Twists help rotate and lengthen your spine and can be performed sitting in a chair or while lying or sitting on the ground. Begin on your back and bring your knees up to your chest. Gently allow your legs to fall to one side and turn your torso in the opposite direction, extending your arm. Breathe in this position for 30 seconds and then repeat on the other side.
You can do this stretch sitting by raising your arms and twisting gently from your torso. If seated in a chair, you can grip the arm of the chair with one hand and put the other hand on the opposite leg. Extend your spine on the inhale and twist a little further on the exhale. Repeat on the other side.
Addressing the Emotional Root of Back Pain
Last but not least, there’s evidence that back pain may originate in, and is certainly exacerbated26,27 by, psychological or emotional issues. The late Dr. John Sarno, a professor of rehabilitation medicine, gained notoriety using nothing but mind-body techniques to treat patients with severe low back pain.
His specialty was those who have already had surgery for low back pain and did not get any relief. This is a tough group of patients, yet he claimed to have a greater than 80% success rate using techniques like the Emotional Freedom Techniques (EFT).
When anger, fear, frustration or rage are suppressed, your brain redirects the emotional impulses to restrict blood flow to certain parts of your body, thereby triggering pain. This pain acts as a distraction from the emotions you don’t want to feel or think about.
As noted by Sarno in the documentary “All the Rage” — a four-minute trailer of which is included above — “I tell [my patient] what’s going on, and lo and behold, it stops hurting.” The “what” that is going on is not a physical problem at all — it’s emotions: anger; fear; frustration; rage.
When these kinds of emotions are suppressed, your brain redirects the emotional impulses to restrict blood flow to certain parts of your body, such as your back, neck or shoulders, thereby triggering pain. This pain acts as a distraction from the anger, fear or rage you don’t want to feel or think about.
The pain essentially acts as a lid, keeping unwanted emotions from erupting. You may feel anger at the pain, but you won’t have to face the fact that you’re actually angry at your spouse, your children or your best friend, or that you hate your job, or the fact that you feel taken advantage of.
As noted by Sarno, working hard and constantly trying to do everything perfectly to keep everybody around you happy, “is enraging to the unconscious mind.” The term Sarno coined for this psychosomatic pain condition is “tension myoneural syndrome,”28 and he firmly believed most people can overcome their pain by acknowledging its psychological roots.
While many of Sarno’s patients got well without psychiatric help, he would often recommend seeking out a psychotherapist to explore repressed emotions, or to take up journaling to put your feelings on paper.
Another doctor who believes resolving suppressed emotions is key for those with chronic back pain is Dr. David Hanscom, an orthopedic surgeon. He prescribes expressive writing as a primary treatment tool for back pain. You can learn more about this on Hanscom’s website, backincontrol.com.29
When to See a Doctor
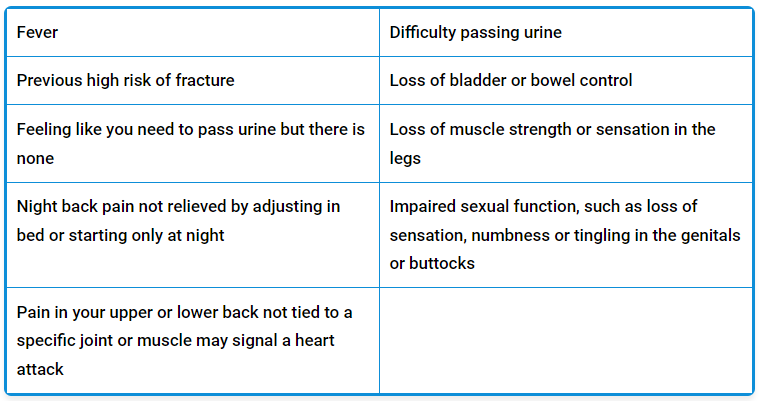
While back pain is rarely indicative of something medically dangerous, if your pain is accompanied by one or more of the following symptoms, a thorough medical checkup would be in order to rule out a more serious problem.30,31,32
Back Pain Is Common, yet Largely Avoidable
Once you understand that back pain is typically the result of poor posture, improper movement, faulty nerve signaling, emotional repression or a combination of these factors, it becomes clear why narcotics and surgery have such high failure rates. They simply don’t address any of the underlying causes.
So, if you’re among those seeking medical care for persistent back pain, I’d advise you to consider your options — several of which I’ve just reviewed — before filling that prescription or going under the knife.
– Sources and References
-
1, 6, 7 Pharmacy Times March 2020; 88(3)
-
2 The Lancet March 22, 2018
-
3 CBS News June 6, 2017
-
4 Journal of Pain October 2018; 19(10): 1104-1112
-
5 Clinical Pain Advisor May 16, 2018
-
8 NBC News, March 21, 2018
-
9 JAMA March 6, 2018;319(9):872-882
-
10 JAMA Psychiatry 2022; 79(1): 13-23
-
11, 12 DW.com June 9, 2022
-
13 A Vogel, August 18, 2015
-
14 Foundation Training
-
15 NST Health
-
16 Vimeo NST Training
-
17 Gokhale Method
-
18 Journal of the American Medical Association 2017;317(14):1451-1460
-
19 Journal of American Medical Association, 2018;1(1):e180105
-
20 Medscape, May 21, 2018
-
21 Reuters Health, May 21, 2018
-
22 International Research and Philosophy Symposium. Sherman College of Straight Chiropractic. Spartanburg, SC. October 9-10, 2004
-
23 WellBridge Clinic
-
24 HealthyWay July 11, 2018
-
25 Yoga Journal, Poses for Back Pain
-
26 Harvard Health April 25, 2016
-
27 Physical Therapy May 1, 2011; 91(5): 700-711
-
28 Tmswiki.org, Introduction to Tension Myositis Syndrome
-
29 Backincontrol.com
-
30 BBC, March 21, 2018
-
31 Prevention, March 3, 2017
-
32 Cleveland Clinic Journal of Medicine, 2008, 75(8):557
From articles.mercola.com